Shoulder pain is a common musculoskeletal pathology, affecting 15 to 30 percent of the adult population.1 It can originate from numerous causes, including rotator cuff tears, rotator cuff tendinosis, label tears and osteoarthritis, and can contribute to functional disability, decreased range of motion and decreased quality of life for patients.2–4
The axillary nerve (AN), lateral pectoral nerve (LPN) and suprascapular nerve (SN) provide most of the sensory innervation in the shoulder, including pain sensation.5
Limitations of Conventional Management Options6
- Rest, ice and physical therapy are unable to provide long-term analgesic benefit
- Nerve blocks, intra-articular steroids and soft-tissue injections provide an inconsistent and highly variable duration of pain relief
- May not be suitable in some candidates due to age and other comorbidities
 Advantages of Using COOLIEF* Cooled Radiofrequency
Advantages of Using COOLIEF* Cooled Radiofrequency
COOLIEF* Cooled RF can bridge the gap between short-term pain relief treatments and TKA by providing a minimally invasive, non-opioid procedure for knee OA pain.
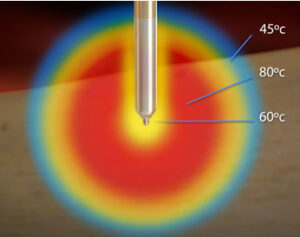
Specifically designed to treat complex anatomy of variable nerve courses, COOLIEF* Cooled RF uses water-cooled technology that enables more RF energy to safely deactivate pain-transmitting sensory nerves. This creates a larger, spherical lesion that distally projects 45% or greater beyond the probe’s tip, allowing physicians to approach the target nerve from any angle.
- 60% of patients who received CRFA experienced >50% pain relief, compared to 33% of standard radiofrequency patients.
- Demonstrates up to 24 months pain relief with improved physical function and a reduction in opioid medication usage.
- Delivers up to 3.7x more energy than standard RF
Evaluating the Effectiveness of CRFA in Treating Shoulder Pain
A 2020 case series published in The FASEB Journal evaluated the effectiveness of CRFA in treating chronic shoulder pain in 12 subjects. Subjects were evaluated for pain and function at one, three, six and nine months using the Visual Analogue Score (VAS) and Shoulder Pain Disability Index (SAPDI). This study concluded that CRFA is an effective treatment for improving pain and function in patients with chronic shoulder pain through nine months.
9-MONTH RESULTS
VAS Pain Scores for 1- to 9-Month Time Points
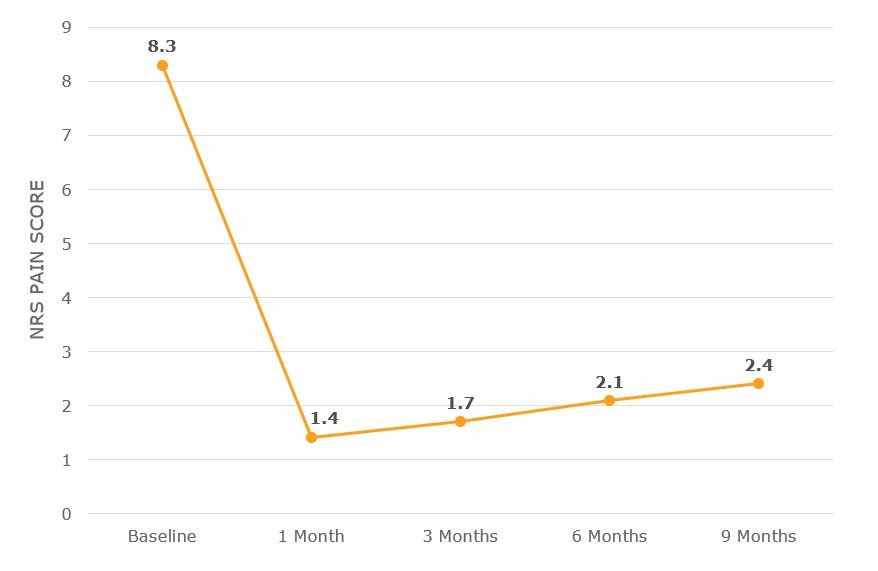
PAIN
Subjects who received CRFA reported a mean decrease of 5.91 points from baseline VAS.
Overall, subjects who received CRFA reported an average VAS decrease of 70% from baseline.
9-MONTH RESULTS
SPADI Function Scores for 1- to 9-Month Time Points
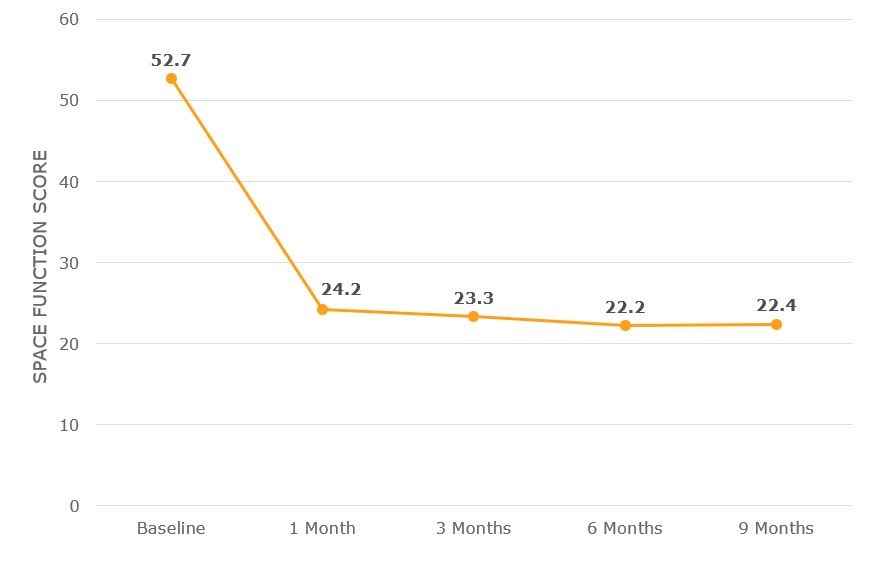
FUNCTION
Subjects who received CRFA reported a mean decrease of 30.31 points from baseline in the SPADI.
Overall, subjects who received CRFA reported an average SPADI decrease of 60% from baseline.
Key Takeaway: CRFA is effective in improving pain and function for subjects with chronic shoulder pain through nine months.

Click here for Instructions for Use
References:
- Orhurhu V, Akinola O, Grandhi R, et al. Radiofrequency ablation for management of shoulder pain. Cur Pain Headache Rep. 2019;23(8).
- Bickelhaupt B, Eckmann MS, Brennick C, et al. Quantitative analysis of the distal, lateral, and posterior articular branches of the axillary nerve to the shoulder: implications for intervention. Reg Anesth Pain Med. 2019;44(9):875-880.
- Ansok CB, Muh SJ. Optimal management of glenohumeral osteoarthritis. Orthop Res Rev. 2018;10:9–18.
- Greenberg DL. Evaluation and treatment of shoulder pain. Med Clin North Am. 2014;98:487–504.
- Laumonerie P, Dalmas Y, Tibbo ME, et al. Sensory innervation of the human shoulder joint: the three bridges to break. J Shoulder Elbow Surg. 2020;29(12).
- Zachariah C, Mayeux J, Alas G, Adesina S, Mistretta OC, Ward PJ, Chen A, English AW, Washington AV. Physiological and functional responses of water-cooled versus traditional radiofrequency ablation of peripheral nerves in rats. Regional Anesthesia & Pain Medicine. 2020 Oct 1;45(10):792-8.

 Advantages of Using COOLIEF* Cooled Radiofrequency
Advantages of Using COOLIEF* Cooled Radiofrequency